Collaborative Care Model
Collaborative Care provides exceptional healthcare in which patients, families, and health professionals are consistently able to co-create care that is meaningful, safe, reliable, resilient, efficient, and exquisitely responsive to the hopes, needs, goals and purposes of everyone involved.
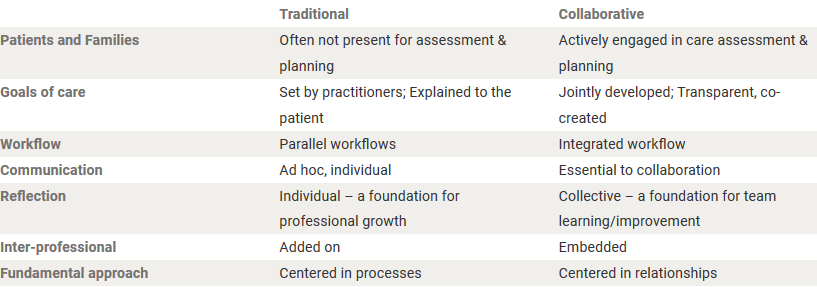
When looking at Traditional Care vs. Collaborative Care, we can highlight some of the changes that we see as explained by the animation.
Key Components of the Model
Daily goals of care
Implemented by discussing team goals and writing them down on a centralized communication. Interpreting the goals achieved creates an open dialogue, builds trust and a rapport between the patient, family and team of providers.
Geographical Localization
By geographically localizing patients during daily workflow at the unit Hospital level, it allows for improved communication with bed control and a faster discharge time for patients.
- Improved communication with bed control allows for the proper placement of patients with different medical teams so that they are placed in the proper areas.
- Faster patient discharge. The charge RN role becomes more important as they work with bed control and coordinate with the bedside nurses so that the appropriate discharges coincide with appropriate admissions of patients onto the unit or teams.
We recognize that implementing this process can be a large hurdle or small one based on the flow and process of the medical units; however, having the right tools in place is a key component for minimizing workflow. This can be accomplished through geographic localization, time management on rounds, patient placement and continuity of care with health care team members.
Patient and Family Engagement
The model fosters an ongoing partnership with patients and families to develop care plans that best meet individual patients’ needs.
Reflections and Communication
Reflection is dedicated time that the team comes together to discuss and reflect on their work together. The goal is to improve patient outcomes, patient experience, communication between all the team members, and overall team function.
Workflow/observation
We have found that keeping a Monday-Friday schedule helps create symmetry for a teaching team that uses a rotational schedule for interns, residents and students. This helps the team stay on task and provides a sturdy foundation for the patients and their families.
Daily Workflow Schedule Example
8:15 - 9:00 a.m. Attending rounds with students
9:00 - 9:15 a.m. Run list with medicine team, case manager, physical therapy and pharmacy
9:15 - 10:30 a.m. Round with full team
10:30 - 11:30 a.m. Continue rounds with partial team (includes: medicine team and all other providers that are still available to meet)
2:00 - 2:15 p.m. Reflection
2:15 - 3:00 p.m. Dedicated teaching time
This schedule allows for changes that may occur over the day while setting specific non-negotiable times for everyone to be on the same page and allows other medical teams and services to be aware of the team’s availability.
