You’ve probably heard of heart disease, cardiovascular disease and maybe even coronary artery disease. Microvascular disease, though, is probably unfamiliar to you — and it’s a disease that women in particular should learn more about.
Dr. Yogamaya Mantha , an interventional cardiologist at the University Health Women’s Heart Center , explains what microvascular disease is and how it impacts women differently from men.
The Role of Microvascular Health
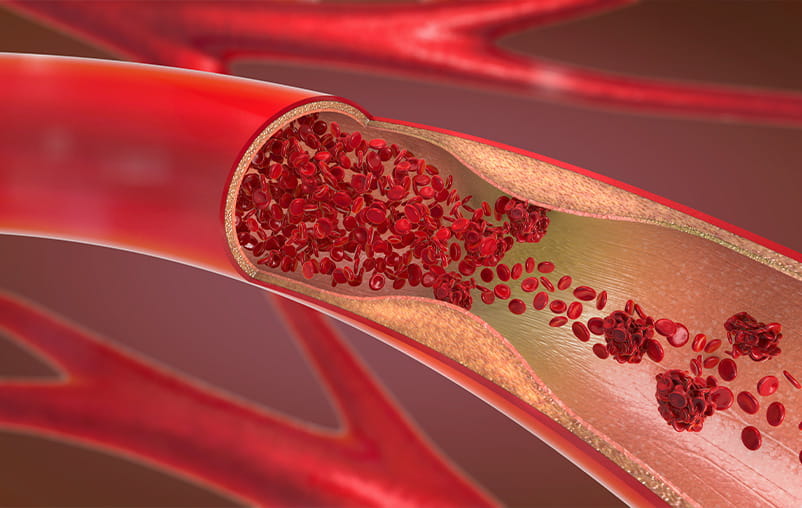
Coronary artery disease occurs when fatty plaque or calcium builds up in the coronary arteries, the large blood vessels that carry blood to the heart. Microvascular disease , on the other hand, affects the tiny blood vessels in the heart.
Although these blood vessels are small, they play a massive role in delivering blood, oxygen and nutrients to heart tissue. When they are damaged or malfunction, blood flow to the heart decreases, leading to chest pain and an increased risk of a heart attack.
Heart disease in general has long been thought of as a “man’s disease,” which we now know isn’t accurate . While men and women share many heart risks, microvascular disease is significantly more common in women.
Recognizing Signs of Microvascular Disease
Microvascular disease is often called “small vessel disease” because of the specific vessels it affects.
“This type of heart disease damages the microvasculature, which is an intricate network of tiny blood vessels in the heart,” said Dr. Mantha.
While some of these blood vessels are no bigger than a strand of hair, they have an outsized role in delivering oxygenated blood to the heart muscle. As the heart is deprived of the oxygen and nutrients it needs, a person may experience:
- Chest pain
- Fatigue
- Shortness of breath with activity
- Sleep disruption, such as (snoring, frequent wake-ups, etc.)
If you experience chest pain, this may last for 10 minutes or longer. It can occur even at rest but often worsens during physical activity or mental stress.
How Microvascular Disease Impacts Women Differently
According to Dr. Mantha, women are at a higher risk of developing microvascular disease due to several factors, including hormonal fluctuations and physiological differences in the female body.
“Women have smaller hearts and narrower blood vessels than men,” said Dr. Mantha. “In a female body, the microvascular blood vessels are even tinier and narrower, which can make it harder for blood to flow through.”
Because women are more prone to microvascular issues rather than large artery blockages, their heart disease often goes undetected.
“Most cardiovascular tests look for blockages in coronary arteries rather than problems with the microvasculature,” Dr. Mantha noted.
Risk Factors for Microvascular Disease
Simply being a woman is a risk factor for microvascular disease. That risk increases with low estrogen levels, appearing either before or after menopause.
Women who have high blood pressure before menopause or who experience intense symptoms during perimenopause or menopause are at higher risk.
While plaque buildup (atherosclerosis) is common in large arteries after menopause, it doesn't usually accumulate in the microvasculature. Instead, damage to these tiny vessels prevents them from dilating (widening) properly, which disrupts blood flow.
Other risk factors can include:
- Certain autoimmune or rheumatologic diseases
- Diabetes
- High blood pressure
- High cholesterol
- Overweight or obesity
- Poor diet
- Sedentary lifestyle
- Smoking
Preventing Microvascular Disease
It is vital for women to talk with their primary care providers about their heart risks, especially after menopause . Checking hormone levels can help determine if low estrogen is a factor so you can take steps to protect your health.
If your provider believes you have a high risk, they will refer you to a heart specialist like Dr. Mantha.
Lifestyle changes to lower your risk:
- Nutrition: Eat a diet filled with fruits, vegetables, lean protein and whole grains. Limit added sugar, saturated fat and sodium.
- Movement: Get at least 30 minutes of moderate physical activity (like brisk walking) most days of the week.
- Habits: If you smoke, work with your provider to quit or learn more about our smoking cessation program . Also, prioritize getting between 7 to 9 hours of sleep each night.
- Management: If you have high blood pressure, cholesterol or diabetes, work with your provider to manage them through medication and treatment.
Diagnosing Microvascular Disease
Doctors typically begin with noninvasive imaging to assess the heart's structure and function without entering the body.
Echocardiogram : This test uses sound waves (ultrasound) to create moving pictures of the heart. It helps doctors evaluate the heart’s overall pumping ability and check for structural issues.
Stress Test with Imaging : This involves exercising or taking medication to raise your heart rate and ultrasound or nuclear imaging to help identify areas of the heart muscle that aren't getting enough blood.
Invasive Testing
If noninvasive tests do not provide a clear answer, your provider may recommend invasive testing. These procedures are performed in a catheterization lab by interventional cardiologists who specialize in microvascular testing, like Dr. Mantha.
Learn more about how University Health Cardiovascular Center is a top performing Cardiac Cath Lab with PCI accreditation.
Coronary Angiogram
In this procedure, a thin tube (catheter) is threaded through a blood vessel to the heart. Contrast dye is injected to make the arteries visible on X-ray, allowing the doctor to rule out major blockages in the large arteries.
Coronary Flow Reserve Testing
Performed during the angiogram, a coronary flow reserve test is considered the “gold standard” for diagnosing microvascular dysfunction. Using specialized software and a pressure-sensing wire, the interventional cardiologist measures blood flow and resistance (coronary flow reserve) within the tiny vessels. This advanced testing provides a definitive diagnosis that standard angiograms often miss.
Treating Microvascular Disease
If you’re diagnosed with microvascular disease, your treatment plan will focus on alleviating your symptoms and preventing serious health issues. This may include medications such as:
- Antiplatelets to prevent blood clots
- Beta-blockers, ACE-inhibitors or calcium channel blockers to lower blood pressure and relax blood vessels
- Nitroglycerin or nitrates to alleviate chest pain
- Ranolazine to ease chest pain by altering electrolyte levels such as sodium and calcium
- Statins and other medications to lower cholesterol
In persistent cases, cardiac rehab and EECP (enhanced external counter pulsation therapy) may be recommended. EECP is a noninvasive therapy that stimulates blood vessels to develop new branches and improves blood flow to the heart, helping to relieve chest pain.
Heart Care at University Health
In San Antonio, Texas, the University Health Cardiovascular Center offers advanced, comprehensive heart care to adults across South Texas. From prevention to diagnosis, you can expect an expert multispecialty team of heart and vascular specialists right by your side.
Women’s Heart Center
As part of the Cardiovascular Center, the University Health Women’s Heart Center provides specialized heart care for women at all ages and stages of life. Our team of experts, including Dr. Yogamaya Mantha , recognize that women face unique risk factors and life situations — and every service we offer takes that into account.
Visit our website to learn more about women’s heart care at University Health or call 210-743-8201 for more information.